Published online Feb 26, 2015. doi: 10.4330/wjc.v7.i2.101
Peer-review started: September 19, 2014
First decision: October 14, 2014
Revised: November 9, 2014
Accepted: November 17, 2014
Article in press: November 19, 2014
Published online: February 26, 2015
Pulmonary arterial dissection is an uncommon but usually a deadly complication of chronic pulmonary hypertension. A 26-year-old female patient was admitted to our clinics with sudden dyspnea and chest discomfort one hour after giving birth to twins by vaginal delivery. An echocardiography was performed with a pre-diagnosis of pulmonary embolism. However, echocardiographic examination revealed a dilated main pulmonary artery and a dissection flap extending from main pulmonary artery to left pulmonary artery. In summary, in this report, we described a very rare case of pulmonary artery dissection in a pregnant patient with a previously un-diagnosed patent ductus arteriosus without an obvious rise in pulmonary artery pressure and reviewed the relevant literature.
Core tip: A 26-year-old female patient was admitted to our clinics with sudden dyspnea and chest discomfort one hour after giving birth to twins by vaginal delivery. Dilated main pulmonary artery and dissection flap extending from main pulmonary artery to left pulmonary artery were found in echocardiographic examination, there after, pulmonary dissection was confirmed by a computed tomography and the patient underwent surgery. In summary, in this report, we described a very rare case of pulmonary artery dissection in a pregnant patient with a previously un-diagnosed Patent ductus arteriosus without an obvious rise in pulmonary artery pressure and reviewed the relevant literature.
- Citation: Yaman M, Arslan U, Ateş AH, Aksakal A. Pulmonary arterial dissection in a post-partum patient with patent ductus arteriosus: Case report and review of the literature. World J Cardiol 2015; 7(2): 101-103
- URL: https://www.wjgnet.com/1949-8462/full/v7/i2/101.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i2.101
Pulmonary arterial dissection is an uncommon but usually a deadly complication of chronic pulmonary hypertension. However, with the development of diagnostic and therapeutic interventions in recent years, a few reports in surviving patients with pulmonary artery dissection have been reported[1].
Patent ductus arteriosus (PDA) is a congenital anomaly caused by a failure to close of a fetal vessel which connects the pulmonary artery directly to the ascending aorta after birth. A rare but lethal complication of PDA is pulmonary artery dissection and dissection usually occurs as a result of chronic pulmonary arterial hypertension associated with PDA and is typically seen in patients with Eisenmenger’s syndrome[2-5]. In this report, we described pulmonary artery dissection in a pregnant patient with a previously un-diagnosed PDA without an obvious rise in pulmonary artery pressure.
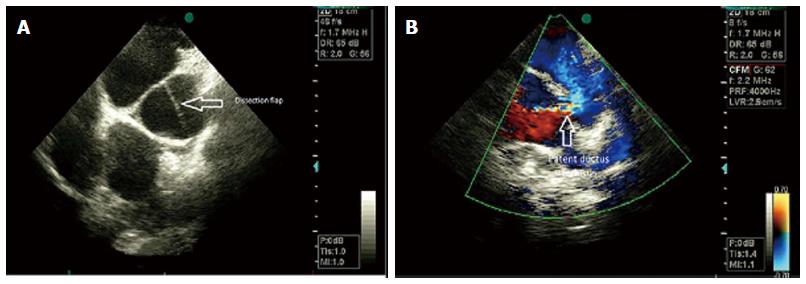
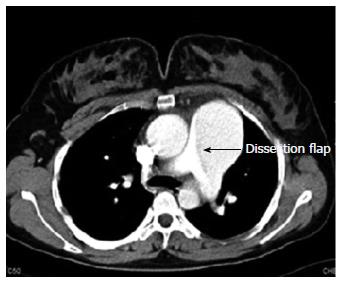
A 26-year-old female patient was admitted to our clinics with sudden dyspnea and chest discomfort one hour after giving birth to twins by vaginal delivery. She had no previous medical history. On physical examination, her blood pressure was 100/60 mmHg and pulse rate was 125/min. The ECG was consistent with sinus tachycardia. An echocardiography was performed with a pre-diagnosis of pulmonary embolism. However, echocardiographic examination revealed a dilated main pulmonary artery and a dissection flap extending from main pulmonary artery to left pulmonary artery (Figure 1A). Besides, in suprasternal and parasternal views, a PDA was observed (Figure 1B). Moderate tricuspid regurgitation was present with a peak continuous wave velocity 2.7 m/s. A thorax computed tomography examination was then performed which showed the dissection flap and the false lumen in the main pulmonary artery (Figure 2). The patient underwent emergent surgery after clarifying the diagnosis. A Dacron graft was positioned in the main pulmonary artery and the PDA was closed. She was discharged from the hospital at the 12th post-operative day. She was in a good clinical condition and asymptomatic at her regular policlinic controls.
PDA is a congenital heart disease resulting from the postnatal closure defect of the ductus arteriosus. It represents 5%-10% of all congenital heart diseases, with a female-to-male ratio of 2:1. Delayed treatment may lead to certain complications including pulmonary hypertension, Eisenmenger’s syndrome, congestive heart failure, and infective endarteritis. Though rare, pulmonary artery dissection may also be included in the above list of complications.
Posing a high mortality risk, pulmonary artery dissection results from congenital heart diseases, pulmonary hypertension and cardiac interventions[1]. Right heart endocarditis, amyloidosis, trauma and severe atherosclerosis may also result in pulmonary artery dissection[6]. The most common cause is pulmonary hypertension associated with congenital heart disease. Interestingly, in our case, the patient did not have pulmonary hypertension.
The main pulmonary artery is involved in 80% of the pulmonary artery dissection cases. However, isolated cases with right or left pulmonary artery involvement can also be seen. Localized small dissections are rare. Because rupture causes cardiogenic shock and sudden death, diagnosis is rare in the living subject and pulmonary artery dissection is frequently detected in autopsy[5]. Khattar et al[1] stated that only 8 (12.6%) out of 63 cases were diagnosed to have pulmonary artery dissection while living, and that 34 (53.9%) of the cases had congenital heart disease[1]. In our case report, pulmonary dissection was reliably diagnosed by transthoracic echocardiography, and thereafter the diagnosis was confirmed by computed tomography examination.
Pulmonary artery dissections usually occur in patients with medial degeneration and pulmonary arterial dilatation due to chronic increases in pulmonary arterial pressures[7-10]. Medial degeneration is a common cause of weakened pulmonary arterial wall and dilatation of the vessel and if intravascular pressure and shear stresses increase due to pulmonary hypertension, intimal tear may develop and cause dissection in the arterial wall. In our case, we thought that pregnancy predisposed the patient to dissection due to weakening of the connective tissue and pulmonary dissection occurred during difficult twin labour which increases venous return and blood pressure in the alreadily dilated pulmonary bed due to PDA.
In aortic dissection, the false lumen usually extends distally and develops a re-entry site. However, in pulmonary dissection, the false lumen usually ruptures causing sudden death of the patient[7-10]. Cardiac tamponade due to rupture seems to be the most common mechanism of death in case of pulmonary dissection[10]. We were lucky because our patient survived this serious clinical situation.
For the first time in literature, we reported a very rare case of pulmonary dissection after giving birth to twins. Presence of PDA without an obvious increase in pulmonary arterial pressures made us think that a transient increase in venous return and pressure during labour caused the dissection to occur. With the development of new imaging techniques providing high quality images in acceptably short time intervals, this mortal disease has become to be diagnosed before death. Moreover, successful repair of pulmonary dissection with surgery has been reported in recent reports including ours. In conclusion, the success of early diagnosis and surgical intervention in pulmonary dissection necessitates an increased awareness of this highly mortal condition.
A post-partum patient with sudden dyspnea and chest discomfort after giving birth was admitted.
Tachycardia and a systolic murmur were found on physical examination.
Pulmonary embolism, aortic dissection.
Echocardiography and computed tomography were used for the diagnosis of patent ductus arteriosus and pulmonary dissection.
Surgical treatment for pulmonary dissection and patent ductus arteriosus closure was performed.
Few reports are present about pulmonary dissection in the literature and this is the first report regarding the presence of pulmonary dissection in a post-partum patient without an obvious rise in pulmonary arterial pressures.
An increased awareness of pulmonary dissection with a view to early diagnosis and corrective intervention is necessary in selected cases.
It is an excellent work.
P- Reviewer: Petix NR, Patanè S, Said SAM S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Khattar RS, Fox DJ, Alty JE, Arora A. Pulmonary artery dissection: an emerging cardiovascular complication in surviving patients with chronic pulmonary hypertension. Heart. 2005;91:142-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 64] [Cited by in F6Publishing: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Zhao Y, Li ZA, Henein MY. PDA with Eisenmenger complicated by pulmonary artery dissection. Eur J Echocardiogr. 2010;11:E32. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Rousou AJ, Haddadin A, Badescu G, Geirsson A. Surgical repair of pulmonary artery dissection. Eur J Cardiothorac Surg. 2010;38:805. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Ay Y, Ay NK, Aydin C, Kara I, Zeybek R. A rare complication of pre-Eisenmenger patent ductus arteriosus: Pulmonary artery dissection. Int J Surg Case Rep. 2013;4:483-485. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Westaby S, Evans BJ, Ormerod O. Pulmonary-artery dissection in patients with Eisenmenger’s syndrome. N Engl J Med. 2007;356:2110-2112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Wunderbaldinger P, Bernhard C, Uffmann M, Kürkciyan I, Senbaklavaci O, Herold CJ. Acute pulmonary trunk dissection in a patient with primary pulmonary hypertension. J Comput Assist Tomogr. 2000;24:92-95. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Shilkin KB, Low LP, Chen BT. Dissecting aneurysm of the pulmonary artery. J Pathol. 1969;98:25-29. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 40] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Lüchtrath H. Dissecting aneurysm of the pulmonary artery. Virchows Arch A Pathol Anat Histol. 1981;391:241-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Yamamoto ME, Jones JW, McManus BM. Fatal dissection of the pulmonary trunk. An obscure consequence of chronic pulmonary hypertension. Am J Cardiovasc Pathol. 1988;1:353-359. [PubMed] [Cited in This Article: ] |
| 10. | Inayama Y, Nakatani Y, Kitamura H. Pulmonary artery dissection in patients without underlying pulmonary hypertension. Histopathology. 2001;38:435-442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 62] [Article Influence: 2.7] [Reference Citation Analysis (0)] |